Hospitalist Burnout and Sociotechnical Factors Contributing to Workplace Stress
Hospitalist Burnout and Sociotechnical Factors Contributing to Workplace Stress
ISE Magazine February 2021 Volume: 53 Number: 2
By Sara Baker Stokes, Richa Kanwar, Saumya Jain, Karthik Adapa, Samantha Meltzer-Brody and Lukasz Mazur
https://www.iise.org/iemagazine/2021-02/html/mazur/mazur.html
National studies have shown that almost 50% of physicians experience some manifestations of burnout. Specialties at the front line of healthcare access, including internal medicine, emergency, and primary medicine, show rates higher than national averages (“Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General U.S. Working Population Between 2011 and 2017,” Tait D. Shanafelt, Colin P. West, Christine Sinsky, Mickey Trockel, Michael Tutty, Daniel V. Satele, Lindsey E. Carlasare and Lotte N. Dyrbye, Mayo Clinic Proceedings, 2019).
Providers with extensive direct patient care, like hospitalists, have been shown to have the greatest risk for burnout. Hospitalists perform a central role in the delivery of patient care in the inpatient setting. While responsible for the general internal medicine care of admitted patients, they attend to a broad spectrum of increasingly complex, higher acuity patients who often have a number of comorbidities. The nature of the care they provide requires working with a broad range of provider-specialists and support staff across the healthcare facility.
This complexity and interdependence with numerous other groups exposes the importance of the sociotechnical systems operating within the inpatient setting. Breakdowns within these systems have a negative impact on hospitalists’ ability to deliver efficient, high quality patient care and potentially in-crease the risk of burnout.
Recent work has focused on work processes associated with health information technology, such as electronic health records (EHRs), as a primary source of providers’ burnout. However, to get a complete picture of all the systemic factors contributing to burnout, a broader sociotechnical approach is required to capture the complexity of the interconnected systems. Therefore, the objective of this study was to assess the levels of burnout among hospitalists and the differences in perceived sociotechnical factors contributing to such burnout.
Methods, participants and data collection
This research was reviewed and approved for exemption by the institutional review board committee at the participating institutions. Hospitalists at two healthcare facilities within a large integrated healthcare system – one an academic medical center, the other a large community hospital – were the target population of this study.
A survey was administered to all hospitalists at the two participating hospitals. The survey instrument was created to gather responses to three components: 1. demographic items, such as sex, age, length of tenure in current position and hospital type; 2. healthcare workplace burnout measures, including the full 22-item Maslach Burnout Inventory (MBI-HSS; see related article at right); and 3. 27 items based on various sociotechnical workplace factors, such as issues related to work processes, organizational culture, efficiency and usability of EHR and other technologies, communications and relation-ships within and outside groups and role clarity.
This survey was administered to all hospitalists at the two participating hospitals. Participants were asked to rate the ex-tent to which they felt the specific workplace factor contributed to their stress, with higher values representing stronger agreement that the factor did contribute to distress.
Data analysis of burnout rates and factors
To understand the extent of hospitalist burnout, we employed three dichotomous definitions of burnout – low, moderate and highly restrictive. Least restrictive is burnout defined by the experience of high levels of at least one manifestation of burnout: emotional exhaustion (EE) >= 27; de-personalization (DP) >= 10; and personal accomplishment (PA) <= 33. Moderately restrictive was burnout defined as experiencing high levels on two manifestations of burn-out. And most restrictive is burnout defined as experiencing all three manifestations of burnout: high on EE and DP, low on PA.
To explore the association between burnout and the perception of socio-technical factors, we used independent two-sample T-test (two-tailed) to identify factors differing significantly as a function of burnout level. Significance level was set at 0.05. The moderately restrictive dichotomous definition was used to perform this analysis as it yielded appropriate sample size within each group: N = 26 with burnout (45%) vs. N = 34 (55%) without burnout.
The overall survey participation rate was 68%, 58 of 85 eligible hospitalists at the academic medical center (67%) and community hospital (71%). Of those responding, 41% were male and 59% female. Their ages: 28% were younger than 35, 45% were ages 35 to 44, 21% were ages 45 to 54, 7% were ages 55 to 64. There were 59% of respondents from the academic medical center, 41% from the community hospital. Their length of tenure in position was 43% with four or fewer years, 35% with five to nine years, 16% with 10 to 14 years and 5% with 15 years or more.

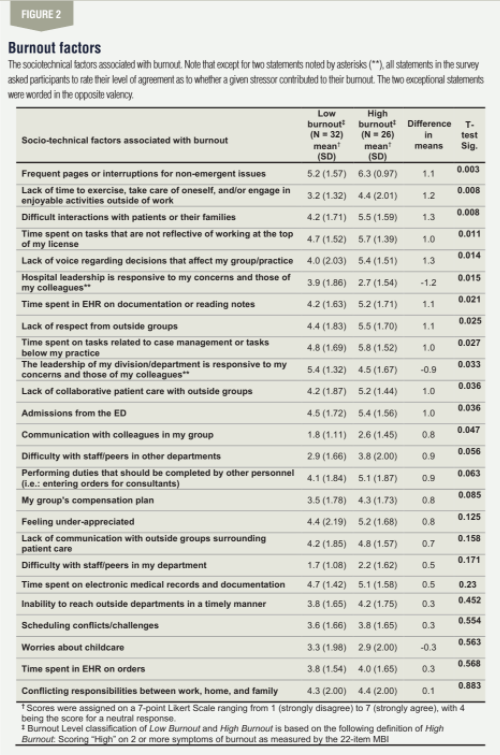
Figure 1 presents the overall and demographic results for hospitalists experiencing high vs. low burnout. The less restrictive definition of burnout (experience one manifestation – i.e., sub-scale, of burnout) yielded burnout rates of 69%. The moderately restrictive definition of burnout (two manifestations of burnout) yielded burnout rates of 45% and most restrictive (all three manifestations of burnout) yielded burnout rates of 24%.Figure 2 presents the overall results including factors differing significantly as a function of burnout level. The following factors were found to differ between hospitalists with and without burnout: time spent on tasks that could or should be performed by others (p < 0.05); suboptimal relationships with other groups (p < 0.05); and frequent interruptions and process-breakdowns were rated as contributing most to hospitalist distress (p < 0.05).
The objective of the study was to understand the extent and nature of burnout among hospitalists providing patient care at a large healthcare system. An additional goal was to assess the differences in perceived sociotechnical factors contributing to burnout in hospitalist with vs. without burnout. Applying the definition of burnout used in the large national physician study, namely the experience of either one or both emotional exhaustion (EE) or depersonalization (DP) as measured by the MBI, 69% of the hospitalists in the current study population fit this definition of burnout, markedly higher than the approximately 50% among general internal medicine providers reported in the most recent national study (hospitalists were not specifically reported), and 52% of hospitalists in the 2014 national study.
Using a somewhat more restrictive definition of burnout as defined by high scores in both EE and DP reduces the percent-age of hospitalists experiencing burnout to 45%, more consistent with the national study. This is worrisome and suggests that rates of burnout are possibly increasing, with 24% of hospitalists experiencing all symptoms of burnout which can lead to adverse events like increased likelihood of medical errors and decreases in quality of care.
Regarding the sociotechnical factors relating to burnout, the factors that had the greatest discrepancy between hospitalists experiencing high vs. low burnout were predominantly characterized as suboptimally implemented roles, such as extensive time spent on tasks that could or should be performed by others, on documentation and extensive/frequent interruptions on non-emergent issues; difficulties in work culture and relationships, such as difficulties with staff/peers in other groups, lack of respect from outside groups or lack of collaborative patient care with outside groups; and lack of support regarding difficult patient/family interactions, responsiveness from group and hospital leadership.
These findings are in line with research reported in the National Academy of Sciences’ recent report on clinician burn-out, expanding on the impact that sociotechnical factors such as professional relationships and social support, organizational culture, excessive workload and suboptimal workflows, interruptions and distractions have on physician well-being. How-ever, these findings are contrary to recent findings by Herbert L. Fred and Mark S. Scheid (“Physician Burnout: Causes, Consequences and (?) Cures,” Texas Heart Institute Journal. 2018) and Mark A. Micek, Brian Arndt, Wen-Jan Tuan and Elizabeth Trowbridge (“Physician Burnout and Timing of Electronic Health Record Use,” ACI open, 2020) indicating that perceptions of work processes associated with health in-formation technology differed significantly based on level of burnout experienced.
Overall, our findings suggest that hospitalists’ burnout is mostly related to workplace roles, relationships and communication with outside groups, and extraordinarily high levels of interruptions and distractions, requiring long-term organizational interventions focused on building trust and collegiality.
There are several limitations of our study limiting the generalizability of our findings. First, we administrated our survey to hospitalists from two institutions with relatively small sample sizes. Another limitation is the construction of the survey relied on the sociotechnical factors identified during town hall meetings with hospitalists articulating workplace factors they were currently struggling with, and therefore may not be comprehensive. Additionally, the response scales employed within the survey varied from section to section. One section of items was on a 4-point scale; others were on a 10-point scale.
Our analyses regarding the sociotechnical factors were limited to differences between groups (low burnout vs. high burnout) within items rather than across items, which would lend much richer analyses of the relationships among the sociotechnical factors. We also tried to address this limitation by computing a transformation of the data to standardize all sociotechnical factors to the same scale; however, issues of scale variability contribute to error in our assessment.
Overall, this study shows that hospitalists are experiencing high levels of burnout, above recent national averages. More-over, sociotechnical factors associated with their experience of burnout tend toward issues with the complexity of their role, their relationships with colleagues in other groups and excessive workloads, interruptions and distractions.



Comments :